Originally published on Carestream Everything Rad http://www.carestream.com/
May 16, 2015 - In Biblical times, Moses parted the red sea; in World War II, the allies landed on D-day; and in Star Wars, the legendary Obi–Wan Kenobi trained the young Jedi to destroy the dark star and save the day.
But today, who or what great event will force health care’s hand so that all health care systems become interoperable and work together seamlessly?
“We have been waiting for EHR interoperability since the dawn of EHRs in the 1960s,1”exclaims Donald Voltz, MD, in a recent article on solutions to making EHRs interoperable. Dr. Voltz is clearly frustrated and with reason. He points out that the average hospital operates competing EHR’s that do not share information, causing confusion and leading to medical errors. There’s really no excuse, he points out. The medical industry has had many opportunities to bring about interoperability with the Health Information Technology for Economic and Clinical Health Act (HITECH) and the Meaningful Use EHR Incentive Program requirements are designed to standardize basic EHR functions. What’s the point of having EHRs if they can’t exchange data from one hospital to the next? Can you imagine if your AT&T phone couldn’t call someone using Sprint or Verizon?
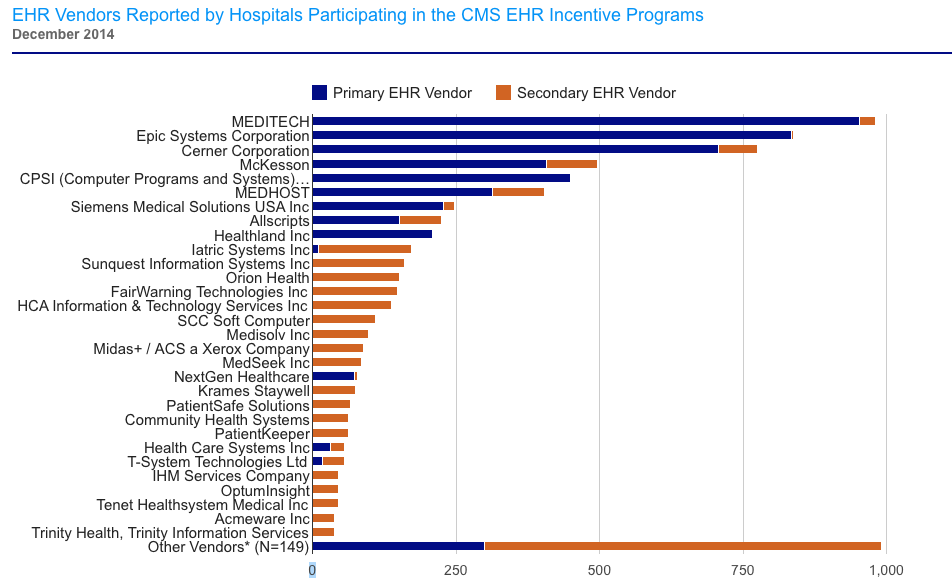
Source: Healthit.gov > Health IT Dashboard > Quick-Stats > Hospital EHR Vendors
So why aren’t these EHRs interoperable yet? Perhaps it’s by design? If so, who’s the man the behind the curtain? The competing hospital networks; the competing vendors; or can we chalk it up to government mismanagement? Or is it simply that their incentives are not aligned?
Getting to the point: Who’s going to save the day?
Maybe it will be the early adopters and self-proclaimed IT innovators in health care—aka, the radiologists. Historically, they have pushed the envelope on embracing new technology, motivated by the need for speed and efficiency when it comes to reading radiology studies. More recently, radiology has made a dramatic shift toward centralizing data as PACS drops the ‘a’ in archiving and morphs into RIS/EHR’s. Others, like David Mendelson, MD, chief of clinical informatics at Mount Sinai Medical Center and principal investigator for RSNA’s Image Share project, have taken the initiative to develop patient portals.
Could personal health records (PHR) play a role in driving EHR interoperability?
PHR’s can do many great things, according to HealthIT.gov. With patient portals your organization can enhance patient-provider communication, empower patients, support care between visits, and, most importantly, improve patient outcomes. Truly transformational? Not there yet.
An independent study, 3 led by Giampaolo Greco, PhD, MPH, assistant professor in the Department of Population Health Science and Policy at the Mount Sinai School of Medicine in New York City, surveyed 2,552 patients, who underwent radiology exams in four academic centers and established online PHR accounts using the RSNA Image Share network. The results showed that 96% responded positively to having direct access to their medical images, and 78% viewed their images independently.
Call it the clinical selfie—who doesn’t want to know what they look like on the inside? The radiologists are certainly on to something when it comes to luring patient into using EHR’s. But are pictures enough to keep them coming back? Even the biggest social media junkies get tired of Instagram. They had to come up with Snapchat—now you see it, now you don’t.
Patient portals are still struggling to engage patients. A recent study, Engaging Primary Care Patients to Use a Patient-Centered Personal Health Record, examined successful portal implementation strategies used by small and medium-sized practices, as well as factors that influenced patients’ use. The results were mixed. The portal, MyPreventiveCare, tried to promote and explain preventive and chronic care to patients. Of the total of 112,893 patients, ranging in age from 18 to 75, nearly 26 percent created an IPHR account; users increased at a rate of about 1 percent per month throughout the entire study period; and patients logged in to the site an average of 3.7 times during the course of the study and spent seven minutes per session. Total patient portal uptake by practice ranged from 22.1 percent to 27.9 percent. The researchers concluded that indeed patients increasingly want to get online and have better access to their doctor—but clinicians need to help them with that.
The next step—better personalize the content. Getting close, but not there yet.
But for patients to truly adopt the portal, they need to own it; not only receive data, but respond to, interact with, and create it themselves. Yes, patients create data by communicating with their health care providers.
The online world is not a monologue; it’s simply another vehicle for everyday dialogue. Patient interaction can close the EHR interoperability gap. Once patients embrace health care IT for themselves, the walls of inoperability will come crumbling down. So, can you guess now the hero is?
- Voltz D. Why I Hope to Help End EHR’s Lack of Interoperability. OpenHealth News. http://www.openhealthnews.com/hotnews/why-i-hope-help-end-ehr%E2%80%99s-lack-interoperability. Posted March 23, 2015.
- What is a patient portal? HealthIT.gov. http://www.healthit.gov/providers-professionals/faqs/what-patient-portal. Posted March 20, 2014.
- Greco G, Patel AS, Lewis S, et al. Patients Take Control of Their Medical Exam Records. Study presented at the annual meeting of the Radiological Society of North America (RSNA). http://www2.rsna.org/timssnet/media/pressreleases/14_pr_target.cfm?id=784. Released December 2, 2014.
- Krist A, Woolf S, Bello G, et al. Engaging Primary Care Patients to Use a Patient-Centered Personal Health Record. 1370/afm.1691Ann Fam Med September/October 2014 vol. 12 no. 5 418-426.
Cristen Bolan, Senior Marketing Specialist, American Organization of Nurse Executives (AONE) – Subsidiary of the American Hospital Association




